Veriben
Veriben™ Provider Communication Solutions
Provider coordination is essential for patient care. Answering basic provider questions over the phone is not.
The Veriben™ solutions give providers relevant claim and eligibility data on your behalf, so that you can reduce provider calls and work more productively.
Schedule a demo to see how you can use Veriben™ to efficiently communicate with providers.
Remove Bottlenecks, Build Scalability
Don’t let basic claim and eligibility calls bottleneck your provider contact centers and constrain the productivity of your team. Use the full Veriben™ lines of defense to:
Prevent basic claim and eligibility calls from reaching your contact centers
Refocus your team on complex provider needs
Scale your provider communications as your business grows
Drive provider self-service
As you bring on more business and interact with more providers, Veriben™ will be your technical right hand, answering the basic claim and eligibility questions for you. This will allow your team to work more productively and your provider operations to scale more effectively.

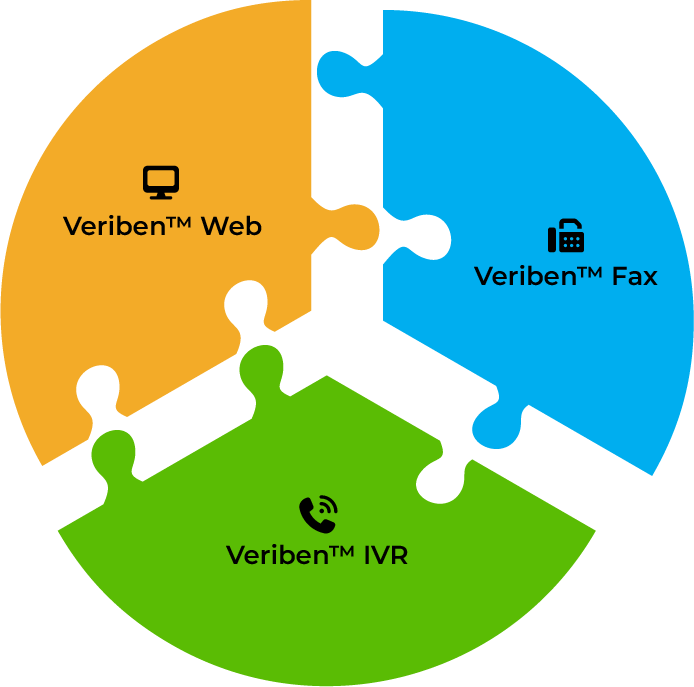
Veriben™ Provider Communication Solution Set
The Veriben™ tools let you communicate basic claim and eligibility details to providers without your team’s manual involvement.
Veriben™ Web
Your digital provider service desk.
Providers check claim status and patient eligibility online without having to log in.
Veriben™ IVR
Your automated call center.
Providers use Interactive Voice Response to request and listen to claim status and eligibility over the phone.
Veriben™ Fax
Your hands-free transmission of data.
Providers request and automatically receive claim status and eligibility via fax.
When used together, the Veriben™ solution set helps you minimize provider calls and maximize your team’s productivity.
Don’t let basic claim and eligibility calls slow your provider coordination and erode your productivity.
Schedule a Demo to use Veriben™ to streamline your provider communications.

