Part 1 of our Online Enrollment FAQ talked about the configurability that enables Payers to create targeted online experiences and workflows for various enrollment scenarios, from open enrollment to an address change.
In this portion of the FAQ, we’ll dig deeper into the end user experience and how HPS’ Online Enrollment can facilitate smooth and seamless business processes.
In Part 1, we left off talking about the Employer-specific business rules that can be configured for their enrollment. Beyond those rules, what else does the enrollment do to make the online experience targeted to the member?
The business rules we talked about previously will control and display the benefit options specific to the Employer. However, the online enrollment also has built-in business rules that will control coverage display based on the member’s eligibility. For example, let’s say a member has filled out his demographic details and he is a single member. When he gets to the coverage page, the portal will know the member is single and therefore won’t let the member pick a family plan or employee + spouse plan. This helps the member quickly identify what plan is right for him and get through the enrollment process efficiently.
Speaking of “getting through” the enrollment process, enrollment is notorious for being a confusing and painful process for the average enrollee. What does HPS’ Online Enrollment do to make the enrollment process as painless as possible?
There are lots of “little things” that go a long way for helping the members. For example, if we’ve already got the member’s eligibility details on file, we’ll pre-populate those details into the enrollment forms so the member doesn’t have to fill them out from scratch. If we have their dependent eligibility details on file, we’ll pre-populate those too. Also, when doing an annual enrollment, the member will see the benefits he’s currently enrolled in so he’s got a reference as he selects next year’s coverage. In addition, when a member is enrolling in life or disability, the portal will pre-populate the dependent details into the beneficiary section to reduce the amount of data entry. All these things add up to big time savings for the member.
What happens if the members have questions as they’re going through the enrollment process? How are those addressed?
The online enrollment has several tools clients use to address questions on-demand or to eliminate questions in the first place. For example, we have several content management tools that let clients post instructions or answers to common questions directly on the enrollment web pages. We’ve also seen clients post plan comparison documents and other enrollment-related documents for members to download and use as they’re walking through enrollment. This type of content can be targeted by Employer group, so if it only applies to one Employer, it would only display for members of that group.
For questions that come up as the member is enrolling, we have clients who use online live chat to address those. On every page of enrollment, there is a “Chat With Us” button that displays. If the member has a question, she can click the chat button and send her question to the Payer or Eligibility Department. That party will then be able to instant message with the member to address their question so the member can complete their enrollment.
We’ve been focusing a lot on the member experience side of this. How are things on the Payer side of things? What happens once these enrollments are submitted?
Enrollments can be submitted by the member, Employer, broker, or even the Payer. As enrollments are submitted, the Payer will receive an email notification that there is a new enrollment available for their review. When the Payer logs in, she can view a list of the new enrollments, which can be sorted by Employer. Then, she can review and approve the enrollments either one-by-one or in more of a bulk fashion. As enrollments are approved, they’re placed in an export file that can be imported by the claim system or whatever system is being used to manage the benefits enrollment.
What types of file exports does HPS produce?
In most cases, we produce an industry-standard 834, but we can also produce a flat file based on the needs of the client.
What’s new with the HPS Online Enrollment?
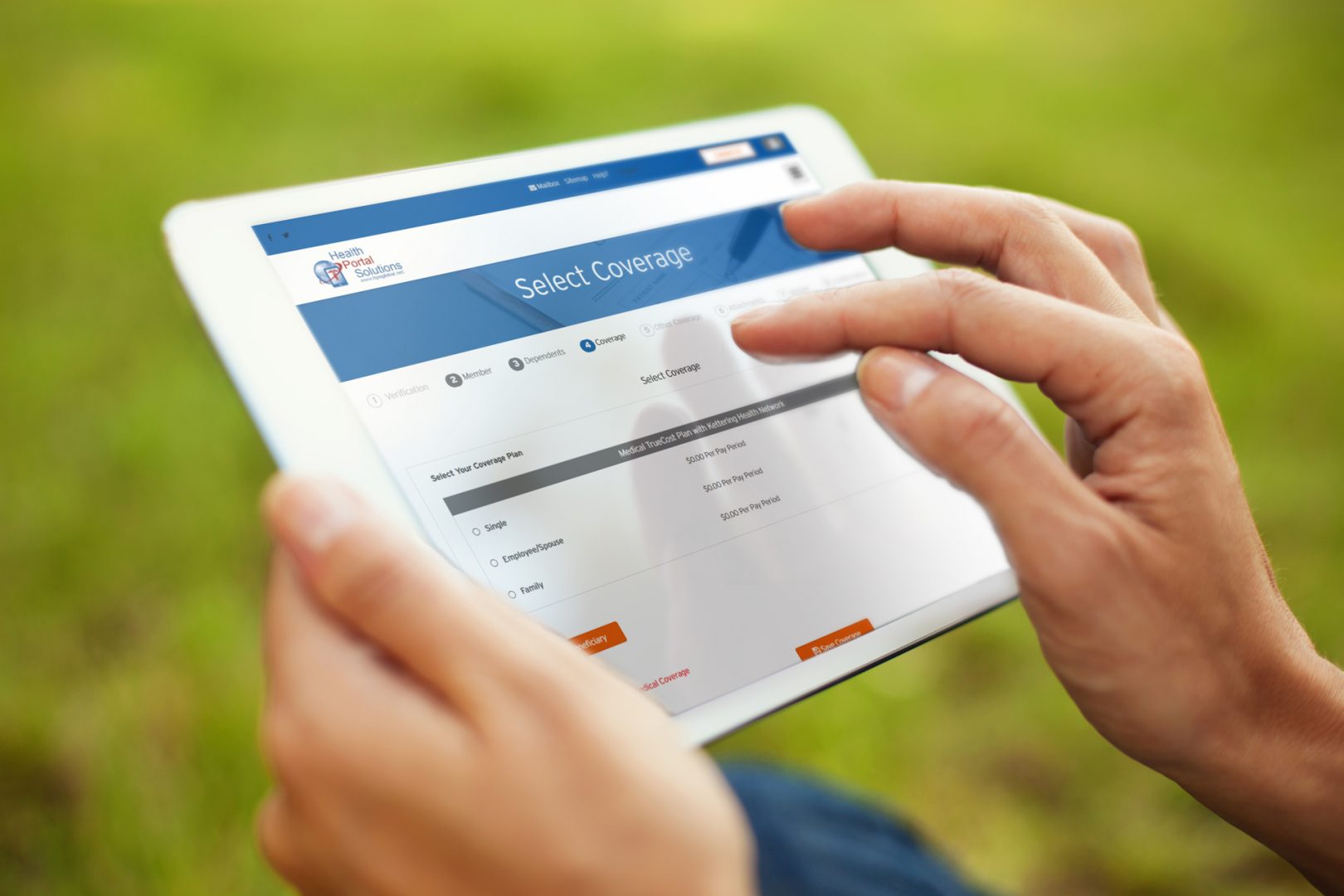
We just released our most enhanced version which is now optimized for mobile. This means online enrollment will automatically resize to fit whatever screen size the member is using. This release also includes a new Enrollment Status Report, which lets Employers and Payers identify which employees still haven’t done online open enrollment. This helps them target enrollment reminders to those members and drive them to use the paperless, electronic enrollment solution offered on the portal.
The configurability of the HPS Online Enrollment makes it a strong business tool for streamlining enrollment and meeting the needs of the members and Employers. To see firsthand how the HPS Online Enrollment can transform your enrollment workflows, contact us.